Gastric cancer

Although the incidence of gastric cancer is decreasing across the globe, including Europe, the burden of the disease is still substantial and will not disappear in the foreseeable future unless effective measures of prevention are implemented. Gastric cancer is the fourth most common cause of cancer-related deaths worldwide and is the fifth most frequently diagnosed cancer.
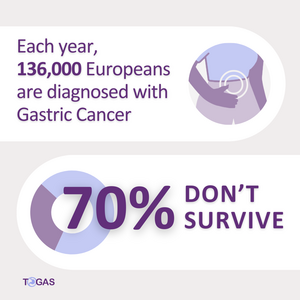
It accounts for over 1 million new cases and almost 800,000 per year deaths globally. Altogether 136,000 new cases were diagnosed in Europe in 2020, accounting for 12.8% of global cases. Considering that the population is ageing both globally and in Europe populations, the absolute number of new cases is expected to grow. In Europe, the annual number of new cases of gastric cancer in 2040 is expected to be 169,000with 124,000 related deaths.
There is broad variation of the incidence of gastric cancer across Europe. Countries with the highest incidence are the Baltic States, Portugal, and Slovenia. Furthermore, the risk of cancer varies among different populations within the same country. Immigrant populations and people of lower socioeconomic status are among the populations with the highest risk. The current wave of immigration from Ukraine could further increase the cancer burden all over the EU, as the Ukraine is considered a high-risk area.
Alarmingly, a trend of increasing incidence of gastric cancer has been reported in younger populations, including in Sweden. By considering the predictions above, a global expert group emphasised already in 2013 the need for immediate implementation of gastric cancer prevention programs
A key issue is the lack of established programs for early detection and prevention of the disease in Western countries. Thus,gastric cancer is usually detected at advanced stage when patients undergo tests to investigate related symptoms. This results in dismal prognosis and poor survival rates. In Western populations, five-year survival rates are as low as 25-30%, in Europe even 19-30%6.
In contrast, 10-year survival in in Japan, where a screening program has been running for decades, has recently reached 58.9%. Early detection is crucial to facilitate minimally invasive treatment modalities (mainly endoscopic resection) and thus lower mortality and morbidity. On the other hand, effective primary prevention is currently only considered to be achievable by early eradication of H.pylori infection of the stomach.
 CONFERENCE
CONFERENCE